This workstream aims to improve and accelerate detection and surveillance of risk among people who use substances, resulting in timely interventions to reduce drug and alcohol morbidity and mortality through data collection at public health, service and individual levels by using innovative data driven technologies, synthesis and predictive modelling.
-

Longitudinal national and area-based drug death profiles
Detailed repeated analyses of drug-related deaths, provide a rich characterisation of the personal, clinical, social, and substance-related factors driving drug deaths in Scotland, and how they continue to evolve over time.
-
Multimorbidity in the context of harmful alcohol use
Dr Nina MacKenzie is a PhD Fellow on the Multimorbdiity PhD Programme for Health Professionals funded by the Wellcome Trust. She is exploring factors associated with, and outcomes from, multimorbidity in the context of harmful alcohol use in Scotland…
-

Chronic opioid use and cardiovascular disease
Chronic opioid exposure (COE) is increasingly recognised as a risk factor for cardiovascular disease (CVD). This PhD in Addiction Medicine, lead supervisor Professor Alex Baldacchino, is exploring the association between COE and atherosclerotic CVD. The goal is to inform prevention and early detection of CVD among people who use opioids including heroin and fentanyl…
-
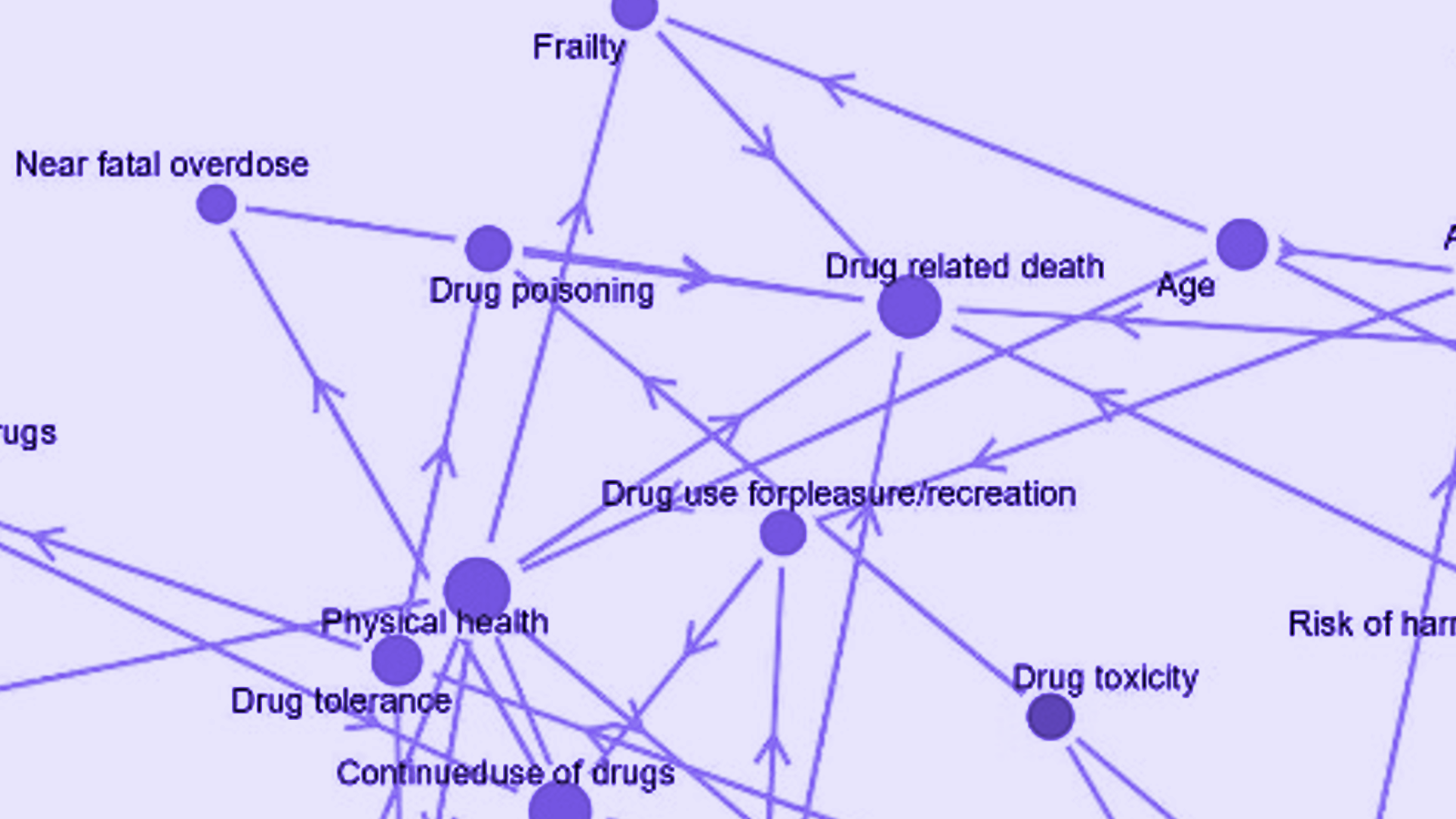
Complex system structures related to drug deaths in Scotland
Funded by the Scottish Government’s Drug Deaths Taskforce, this project took a complex systems approach to understand drug-related mortality. We modelled connections between health conditions, social experiences, and broader political factors through analysis of large linked datasets and focus groups with stakeholders including those with lived/living experience.
-

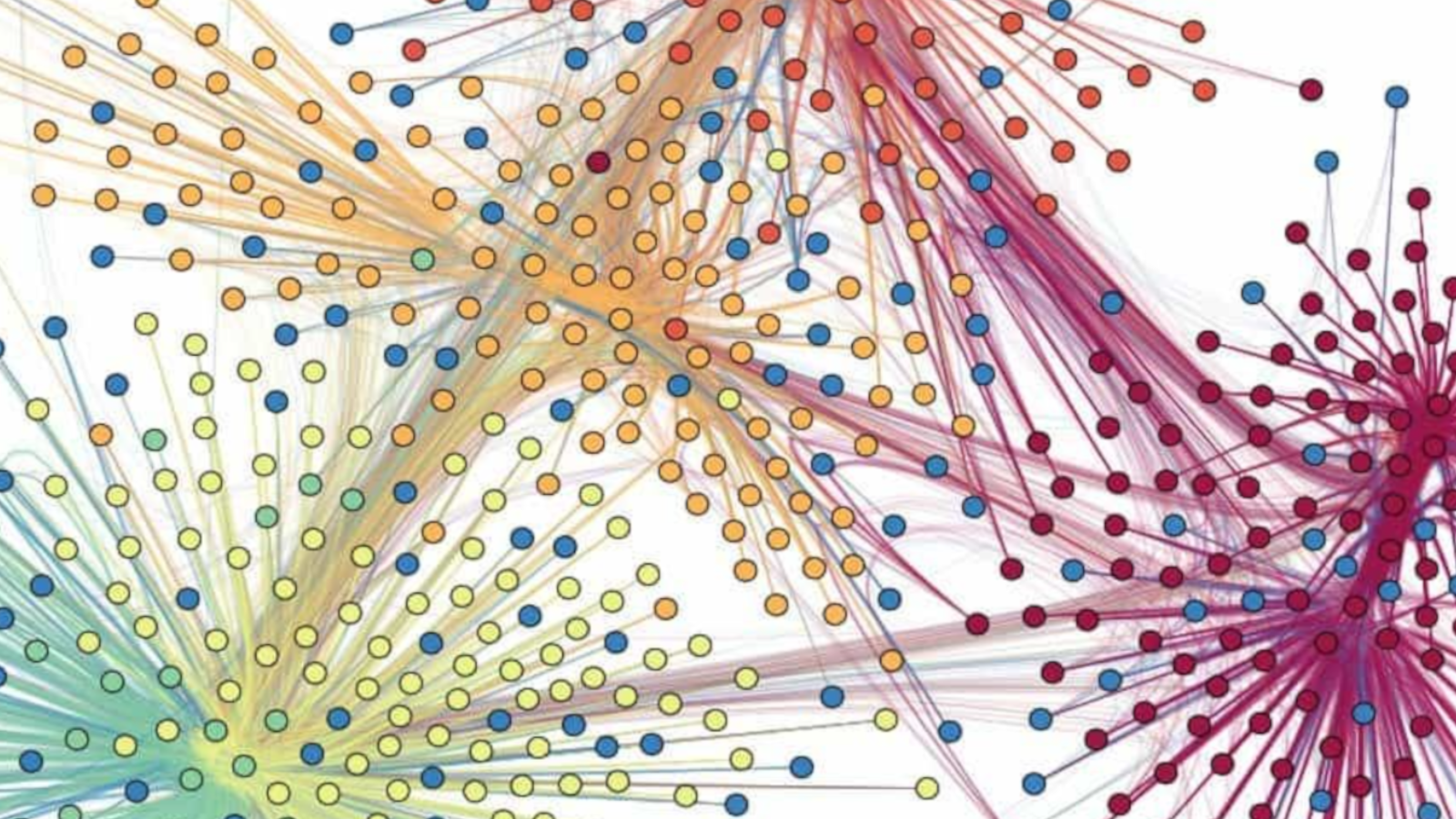
World Addiction Medicine Reports
This protocol outlines ISAM-GEN’s global longitudinal survey initiative, engaging 354 experts from 78 countries and 43 addiction societies. It aims to monitor evolving addiction trends, treatment coverage, emerging needs, and barriers by surveying addiction professionals, programmes, and stakeholders, fostering international collaboration in addiction medicine research and service improvement.
-

Categorising alcohol consumption using primary care health records
Analysis of almost 19,000 Scottish patients in the UK Biobank supported development of a rule-based, multiclass algorithm to classify alcohol consumption based on primary care health records. Results have potential to improve identification of people with harmful consumption and to reduce administrative burden on general practitioners.
-

Alcohol treatment adherence, morbidities & mortality
Acomprosate is an anti-craving medication used to treat severe alcohol dependence. This study explored outcomes among people with poor adherence including medical and psychiatric admissions and mortality. Adherence was suboptimal – only 6% took medication as prescribed at 6 months following initiation. Low adherence was associated with significantly higher risk of death and morbidities within…
-

Opioid use disorder treatment: follow-up & economic analysis
This study compared methadone and buprenorphine/naloxone (Suboxone) for opioid replacement therapy in 237 individuals in Scotland. Over two years, no significant differences were found in retention or healthcare costs. Findings suggest buprenorphine/naloxone is a cost-neutral alternative to methadone, with similar treatment outcomes and potential to support informed clinical choice.
-

Effect of alcohol brief interventions in A&E
nvestigating the impact of Alcohol Brief Interventions (ABIs) in Accident & Emergency (A&E) departments using data informatics methodology involves analyzing patient data to assess the effectiveness of these interventions in reducing subsequent healthcare utilization and associated alcohol-related issues. This approach links patient data from A&E visits with various datasets to track long-term outcomes, such as…
-

Opioid prescribing, pain, and benzodiazepine co-prescribing
This study examined opioid prescribing trends in Scotland from 2003 to 2012, revealing a sharp increase in strong and weak opioid use, with 18% of the population receiving opioids in 2012. Prescribing was higher in deprived areas, often included benzodiazepines, and was significantly associated with pain severity and regional variation.
-

Comparing accidental vs. intentional drug overdose in Scotland
This study analysed drug-related deaths in Scotland in 2003, comparing accidental and intentional overdoses. Those who intentionally overdosed were older, more often female, and had more stable social circumstances. Differences in clinical and social histories highlight the diversity of the drug death population, informing more targeted prevention strategies.
-

Clinical information recording in drug deaths
This study examined case files of individuals who died drug-related deaths in Scotland in 2003, finding over 70% had contact with services in the prior six months. Despite this, key clinical data—such as psychiatric history and blood-borne virus status—were often missing. Improved recording and monitoring could aid prevention efforts.
-
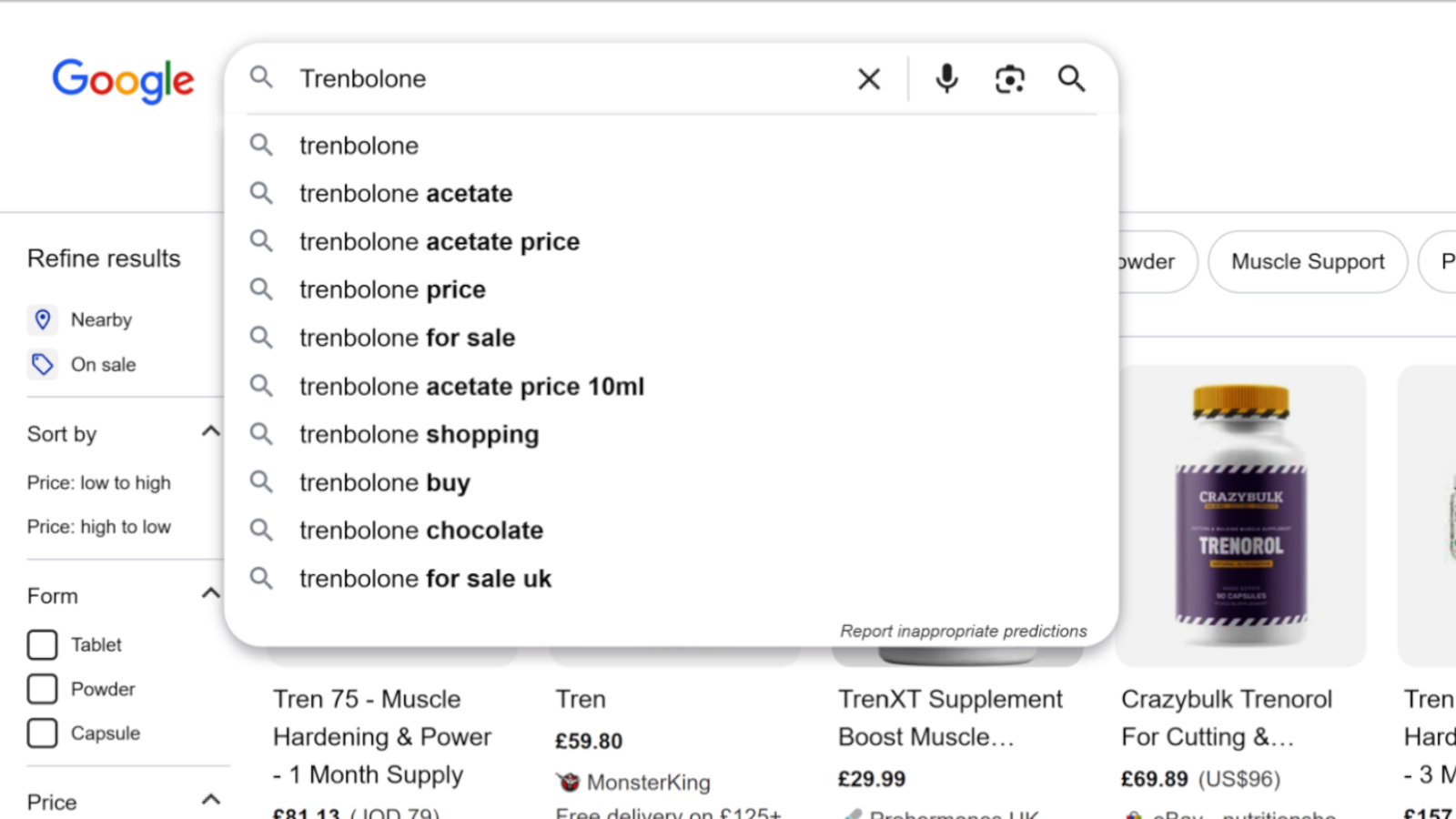
Tracking online interest in anabolic-androgenic steroids
This study explored the use of Google Trends to assess patterns in anabolic steroid interest in the UK. Clear seasonal trends were found for most compounds, with peaks in spring and early summer. While search data cannot confirm use, it may offer valuable, real-time insights to complement traditional surveillance methods and inform harm reduction efforts.
